Industry Briefing #17
Healthcare industry highlights
- Reading time
- 1 min
- Words
- The Briefing
- Published date
- September 9, 2024
The Briefing keeps consultants ahead by unpacking essential trends and emerging questions they can answer through market research.
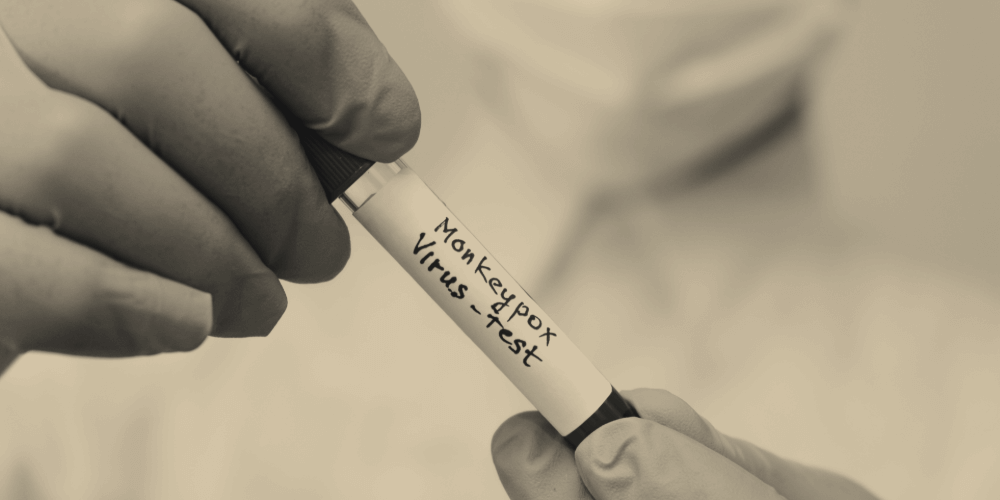
On this week’s issue: Mpox is now a global emergency due to an outbreak in Africa. Cancer research is advancing prevention and survivor support. Pharmaceutical companies are innovating direct-to-consumer models, while food prescription programs provide fresh produce to those in need. Healthcare organizations are adopting AI to streamline documentation.
Questions to Stay One Step Ahead
From obesity to viruses, there are many global healthcare threats of concern right now. While innovative technologies help providers work more efficiently, social and economic inequities persist, often preventing patients from getting the care and support they need. Moving forward, providers will need to balance these concerns about inequity with operational efficiency.
Questions to consider include:
- Direct-to-consumer care: Are consumers willing to get prescriptions directly from pharmaceutical companies? How much are they willing to spend for this added convenience?
- Mpox: What awareness does the general public have about Mpox in your country? Are consumers willing to contribute to charitable initiatives that support vaccine equity?
- AI-powered records management: Are nurses and clinicians willing to adopt AI technology to manage electronic health records? How much time can these new technologies save?
Interested in launching a study on these topics?
Reach out to Potloc today to jumpstart a market research study for your strategic projects.